Managing health care costs with value-based networks
More employers are choosing networks that promote value-based care, delivering affordability and quality of care.
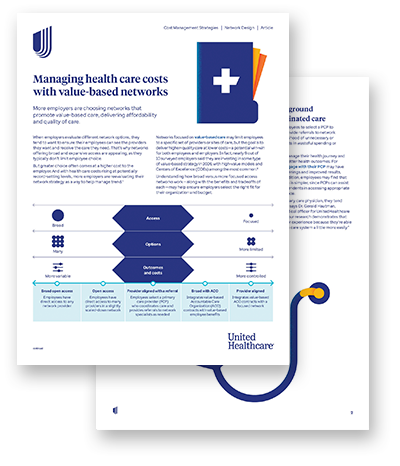
When employers evaluate different network options, they tend to want to ensure their employees can see the providers they want and receive the care they need. That’s why networks offering broad and expansive access are appealing, as they typically don’t limit employee choice
But greater choice often comes at a higher cost to the employer. And with health care costs rising at potentially record-setting levels, more employers are reevaluating their network strategy as a way to help manage trend.1
Networks focused on value-based care may limit employees to a specific set of providers or sites of care, but the goal is to deliver higher-quality care at lower costs — a potential win-win for both employees and employers. In fact, nearly 9 out of 10 surveyed employers say they are investing in some type of value-based strategy in 2026, with high-value models and Centers of Excellence (COEs) among the most common.2
Understanding how broad versus more focused access networks work — along with the benefits and tradeoffs of each — may help ensure employers select the right fit for their organization and budget.
Recognizing that broad access networks can still deliver value
While more employers are considering a shift toward more focused access networks, broad access networks remain the preference for many employees and employers. For example, employers with expansive workforces spread across the nation, or with frequent travel needs, may find a broad access network to be the more appropriate choice. Plus, employers often want to avoid creating friction or disruption for members by forcing them to find a new doctor if their current one becomes out-of-network.
Choosing a broad or open access network doesn’t mean giving up on potential cost savings. Carriers and plans that provide upfront quality and cost information — and prioritize provider search results — may help members make more informed care decisions while still offering freedom and flexibility.
Tiering is another option for cost savings. This approach allows employees access to a wider network but care costs that are varied based on tiered designations — determined by a combination of quality and cost criteria.
Finding middle ground with PCP-coordinated care
When networks require employees to select a PCP to coordinate their care and provide referrals to network specialists, it may reduce the likelihood of unnecessary or inappropriate care that results in wasteful spending or higher costs.
33%
lower health care costs for U.S. adults who regularly see a primary care physician4
When networks require employees to select a PCP to coordinate their care and provide referrals to network specialists, it may reduce the likelihood of unnecessary or inappropriate care that results in wasteful spending or higher costs.
PCPs can help employees manage their health journey and support them in achieving better health outcomes. For instance, employees who engage with their PCP may have better compliance with screenings and improved results, along with lower costs. In addition, employees may find that navigating the health system is simpler, since PCPs can assist them and their covered dependents in accessing appropriate care at the right time and place.
“When members have a primary care physician, they tend to have a lower cost of care,” Dr. Gerald Hautman, chief medical officer of National Accounts for UnitedHealthcare Employer & Individual says. “And our research demonstrates that those members have a better experience because they’re able to navigate a complex health care system a little more easily.”
Prioritizing high-value care for more personalized, cost-effective support
When an employee population has complex health needs or is highly localized geographically, networks that offer more focused access may be a better fit. These types of networks provide employees access to quality based on their unique health needs or situations.
In designing these custom network configurations, carriers often collaborate with local health systems and care providers whose goal is to deliver quality care at lower costs. For instance, UnitedHealthcare offers high-value networks in collaboration with select Accountable Care Organizations (ACOs), Centers of Excellence (COEs) and local health systems.
Collaborations with ACOs
ACOs are groups of doctors, hospitals and other health care providers who voluntarily come together to provide coordinated care to the patients they serve. They hold themselves accountable for the cost and quality of care they offer — helping move the needle on cost management. At UnitedHealthcare, one ACO plan design that encourages the use of physicians and specialists evaluated for quality and cost efficiency generated up to 15% in savings. 4
Collaborations with COEs
COEs — programs that help identify the best available care for complex conditions — may help manage the costs of high-cost claims like cancer treatments. In fact, 84% of surveyed employers said they plan to include COEs in their value-based strategy in 2026.2
COEs may help lead to more accurate diagnoses, fewer readmissions and complications, reduced initial procedure costs and a simplified billing and payment experience.5 Most importantly, COEs may offer higher survival rates and better outcomes.5
Local health systems
Different pockets of the country offer varying health systems, some with more options than others. That’s why collaboration with local health systems may be critical. For example, in areas where there are fewer providers or sites of care, ensuring that the networks are robust enough to meet employees’ needs — or offer alternate options like virtual care — becomes even more important.
Selecting the right network design matters, and UnitedHealthcare is here to help
UnitedHealthcare is constantly evaluating its portfolio of networks to ensure employers have access to options that meet their needs and the preferences of their employees. This includes streamlining the number of network constructs offered and further investing in, evolving or expanding existing networks — to help make the selection process easier for employers, brokers and consultants.