City of Hope in California
We are working on your behalf to renew our network relationship with City of Hope
We are engaged in good-faith discussions with City of Hope (COH) to renew our network relationship. Our goal is to reach an agreement that is affordable for consumers and employers in Southern California, while providing continued, uninterrupted network access to COH.
In the event we are unable to reach an agreement, City of Hope National Medical Center, City of Hope Medical Foundation providers, and COH’s clinical care locations in California will be out of network for people enrolled in the following plans, effective Jan. 1, 2026:
- Employer-sponsored commercial plans
- Medicare Advantage plans, including Group Retiree plans
Facts you should know
We have tremendous respect for City of Hope and the quality care it provides to our members who are living with cancer. That’s why we’re working hard to reach an agreement that is affordable while providing continued, long-term network access to the health system.
We value and appreciate the profound impact COH has on the lives of people living with cancer, including their families. Many of our own employees and their families have been impacted by cancer. We want people to have access to the best care possible.
However, we also have a responsibility to make sure that care is affordable so it’s accessible for all the members we serve.
COH is seeking unsustainable price hikes of more than 25%, which would increase health care costs for consumers and employers in Southern California by nearly $75 million over the next three years
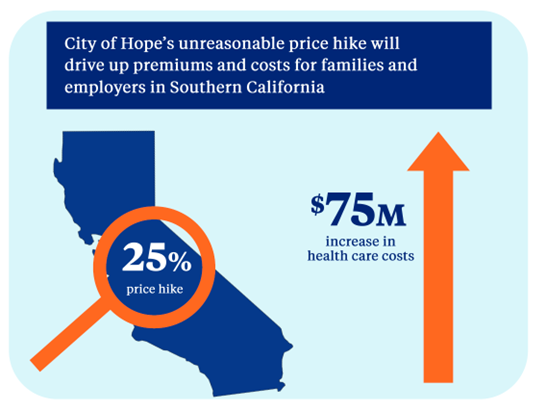
Excessive rate increases drive up overall health care costs, directly resulting in a financial strain for the people we serve.
Agreeing to COH’s proposal would also significantly drive-up premiums and out-of-pocket costs for consumers, as well as the cost of doing business for employers, impacting their ability to offer affordable health care coverage for their employees.
If we agreed to COH’s demands, health care costs would increase for people enrolled in our Medicare Advantage plans while also impacting the benefits these seniors rely on.
We are proposing market-competitive rates that will continue to reimburse COH fairly while slowing the unsustainable rise in health care costs.
Our goal during this negotiation is the same as our members – to help them access the care they need and to make health care as affordable as possible.
City of Hope’s proposed price hikes would significantly drive up the cost of many common cancer treatments and procedures for members who are in the middle of cancer treatment at City of Hope
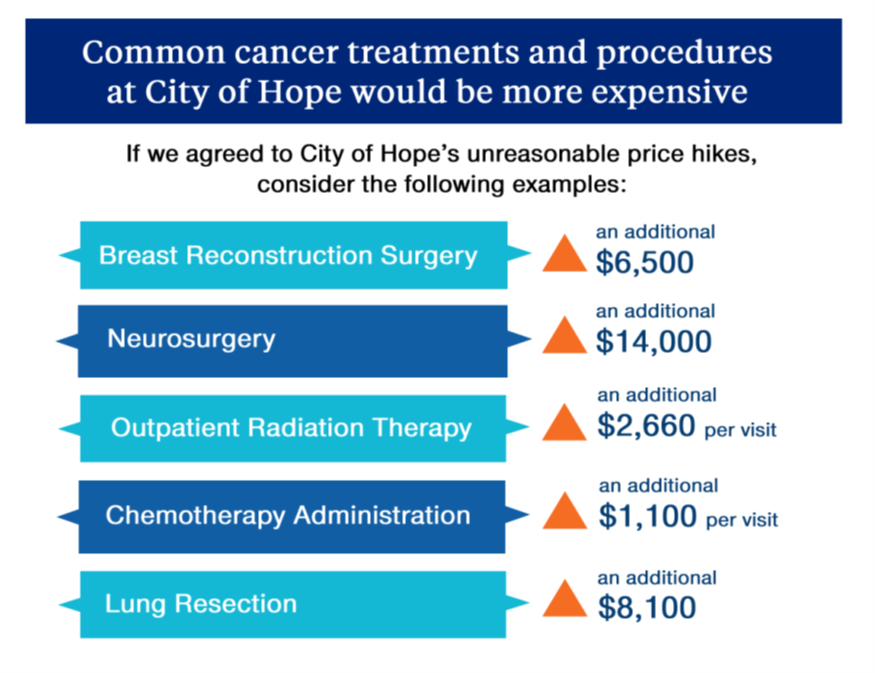
To help illustrate the impact of COH’s proposal, consider the following examples:
- A breast reconstruction surgery would cost more than $6,500 more than that same surgery costs today.
- The average cost of a neurosurgery would increase by nearly $14,000.
- An inpatient gynecological procedure would cost nearly $8,200 more than it does today.
- COH would charge an additional $8,100 for a lung resection and esophagectomy procedure.
- The costs for outpatient radiation therapy would increase by nearly $2,660 per visit and an additional $1,100 more per visit for chemotherapy administration.
- A common colorectal procedure would cost more than $7,800 than it does today.
Employers would face large cost increases if we agreed to City of Hope’s demands
The unreasonable commercial rate increases requested by COH would directly drive-up health care costs for our self-insured customers given that these employers pay the cost of their employees’ medical bills themselves rather than relying on UnitedHealthcare to pay those claims.
Nearly 60% of our employer-sponsored members in California are enrolled in self-funded plans.
Our self-funded employer group customers have charged us with the responsibility of providing their employees access to quality, affordable health care.
We pass any savings from negotiating more competitive rates directly to our self-funded customers, which they could in turn use to hold premiums steady for employees or to lower them in some cases. Employers also use the savings to enhance benefits, increase salaries and help grow their organization.
As the prices for health care continue to rise, employers have less money available to help grow the business through things like investments in new technologies or salary increases for hard-working employees.
As many businesses struggle to attract and retain the employees they need, we are hopeful COH will work with us to reach an agreement at fair, market-competitive rates that will help ensure the people and customers we serve can continue to afford care from the health system.
Frequently asked questions
We have created the following FAQs to ensure you and your family have the information needed regarding next steps as well as details to help meet your health care needs.
We are engaged in good-faith discussions with City of Hope (COH) to renew our network relationship. Our goal is to reach an agreement that is affordable for consumers and employers in Southern California, while providing continued, uninterrupted network access to COH.
We will remain at the negotiating table with COH for as long as it takes to reach an agreement that provides the people we serve continued access to care that is both quality and affordable.
In the event we are unable to reach an agreement, City of Hope National Medical Center, City of Hope Medical Foundation providers, and COH’s clinical care locations in California will be out of network for people enrolled in the following plans, effective Jan. 1, 2026:
- Employer-sponsored commercial plans
- Medicare Advantage plans, including Group Retiree plans
This negotiation impacts members enrolled in the following plans:
- Employer-sponsored commercial plans
- Medicare Advantage plans, including Group Retiree plans
Members enrolled in our Medicare Advantage PPO and Group Retiree plans may receive care from COH as an out-of-network provider, if they are a participating provider that accepts the plan.
If members have a Group Retiree PPO plan, the member’s share of the cost is typically the same as if the provider was part of the network.
UnitedHealthcare Group Retiree members are encouraged to speak with the provider to confirm they will provide care, regardless of their network status.
We understand how important it is to have access to quality care – especially when facing something as serious as cancer. We also recognize and appreciate the relationship people have with their physician is not only important, it’s personal.
In the event COH leaves our network, we want our members to know they will continue to have access to a broad network of cancer centers and oncology specialists across Southern California, including, but not limited to:
- Cedars Sinai Medical Center
- Ronald Reagan UCLA Medical Center
- USC Kenneth Norris Jr. Hospital
- Hoag Memorial Hospital Presbyterian
- University of California Irvine Medical Center
- PIH Health Whittier Hospital
- Huntington Memorial Hospital
For support finding in-network hospitals, members can call the customer care number on their health plan ID card or visit their plan’s website:
- myuhc.com
- myuhcmedicare.com
- retiree.uhc.com for Group Retiree plans
Should we not reach an agreement, our number one priority is providing the people we serve continued uninterrupted access to the care they need. UnitedHealthcare members who are in the middle of cancer treatment at COH are eligible to continue their care at in-network costs.
Continuity of care allows people in the middle of treatment at the time a provider leaves our network to continue accessing care with their provider for a period of time.
Examples of conditions that would be eligible for continuity of care include but are not limited to the following:
- People in active treatment for cancer
- Individuals in ongoing treatment for transplant services
UnitedHealthcare members must apply and be approved for continuity of care.
For information regarding how to apply and whether they might be eligible for continuity of care, members should call the number on their health plan ID card.
In the event of an emergency, UnitedHealthcare members should go to the nearest hospital and will be covered at the in-network benefit level, regardless of whether the hospital participates in our network.
UnitedHealthcare members should always go to the nearest hospital in the event of an emergency. Their services will be covered at the in-network benefit level, regardless of whether the hospital participates in UnitedHealthcare’s network.
For support finding in-network hospitals, members can call the customer care number on their health plan ID card or visit their plan’s website:
- myuhc.com
- myuhcmedicare.com
- retiree.uhc.com for Group Retiree plans