Updated October 31, 2025
Louisiana Children’s Medical Center (LCMC) issued a notice to end our contract and is demanding a more than 40% price hike at its hospitals that would take effect over the next 24 months, including a near 20% rate increase in year one.
Our top priority is to reach an agreement that is affordable for consumers and employers while maintaining continued, uninterrupted network access to LCMC.
Our current contract remains in effect through Oct. 31, 2025. In the event we are unable to reach an agreement, LCMC’s hospitals will be out of network for people enrolled in employer-sponsored commercial plans, including Individual Family Plan (IFP) and UMR, beginning Nov. 1.
LCMC’s physicians are not impacted by the potential termination. They will continue to remain in our network for our employer-sponsored commercial plans, regardless of the outcome of our negotiation. Likewise, LCMC’s ancillary provider locations such as its urgent care centers will also remain in our commercial network on and after Nov. 1.
People enrolled in Medicare Advantage plans, including Group Retiree and Dual Special Needs Plan (D-SNP), as well as our Medicaid plan, are not impacted and will continue to have network access to LCMC’s hospitals, facilities and its physicians.
LCMC’s latest proposal would increase health care costs by more than $113 million for Louisiana families and employers.
While LCMC’s physicians are not impacted by the potential termination, the health system is leveraging the threat of its hospitals going out of network to also obtain substantial price hikes for its doctors.
LCMC’s proposal would significantly drive up premiums and out-of-pocket costs for Louisiana families and employers, and would result in UnitedHealthcare members paying substantially more for care at the health system than other health plans.

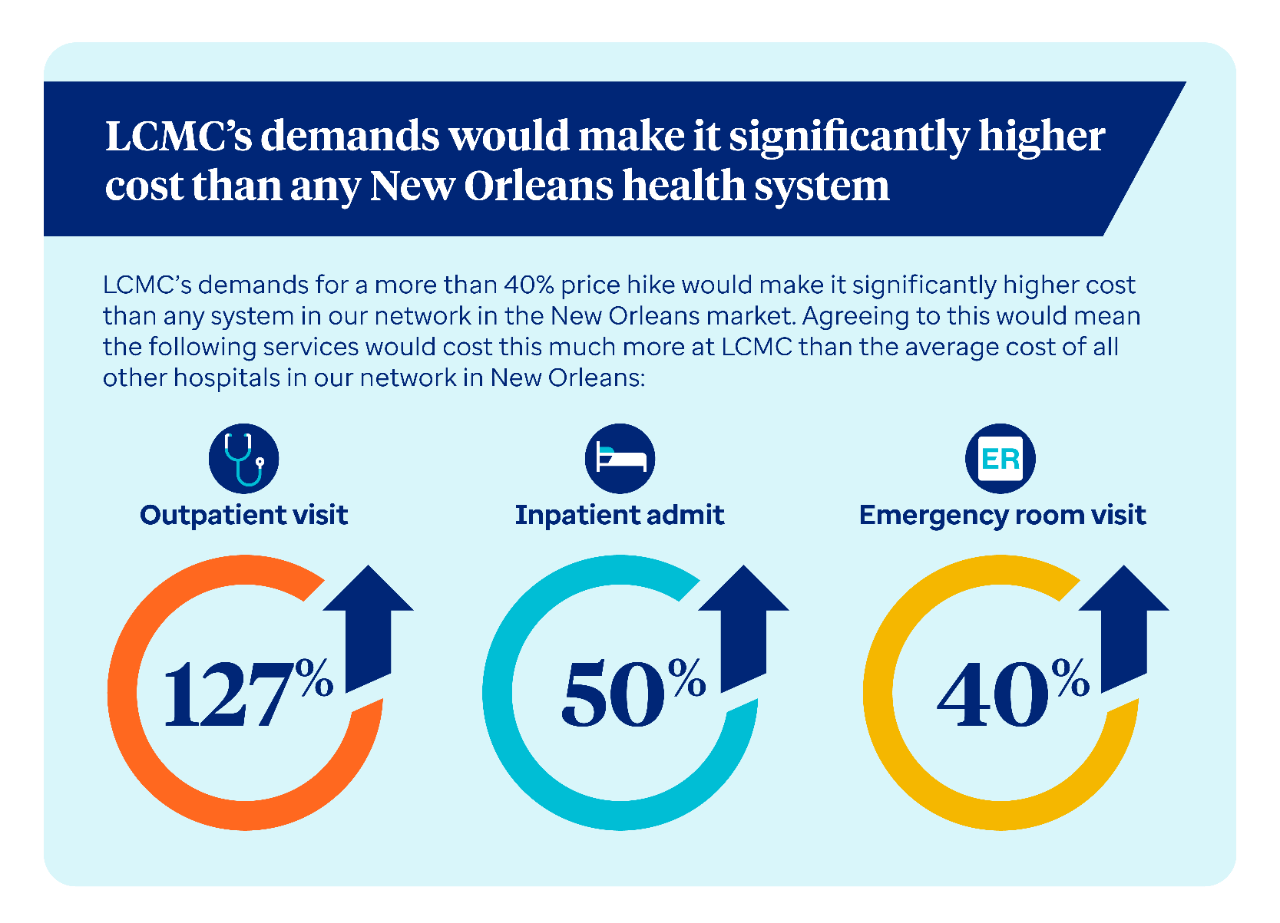
LCMC’s demands for a more than 40% price hike would make it significantly higher cost than any health system in our network in the New Orleans market.
LCMC’s proposed rate increases would mean the following services would cost this much more at an LCMC hospital compared to the average cost of all other hospitals in our network in the New Orleans market:
- The average outpatient visit would be 127% higher cost;
- An inpatient admit to an LCMC hospital would cost over 50% more;
- An emergency room visit would be nearly 40% higher
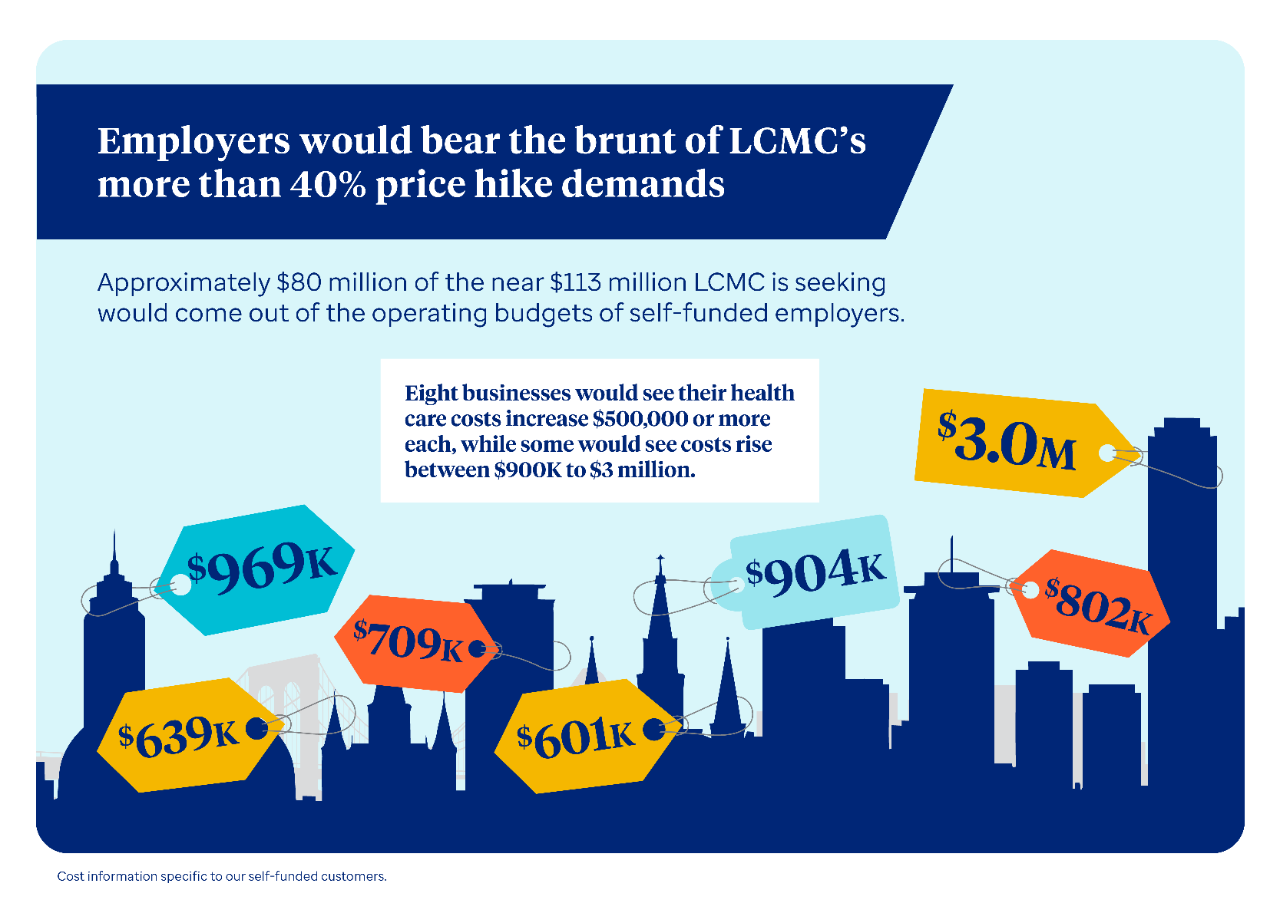
Approximately $80 million of the more than $113 million LCMC is seeking would come out of the operating budgets of self-insured employers.
LCMC’s demands for exorbitant cost increases would directly drive up health care costs for self-insured employers. Eight employers would see at least a $500,000 increase or more if we agreed to the health system’s proposal.
Some of the most heavily impacted employers would see their costs increase between $900,000 to as much as $3 million.
As the prices for health care continue to rise, these employers have less money available to help grow their business through things like investments in new technologies or increase salaries for employees.
LCMC’s proposal would send health care prices skyrocketing for people and employers. Consider how much more the following services would increase in costs at LCMC’s hospitals by Nov. 1, 2027 if we agreed to the health system’s more than 40% price hike demands.
The cost of a C-section would cost approximately $4,800 more than it does today at Lakeview Hospital, Lakeside Hospital and East Jefferson General Hospital. To put this into perspective, a person with a 20% co-insurance would see a near $1,000 increase alone in their out-of-pocket costs for a C-section at one of these three hospitals.
The cost of a C-section at Touro Hospital would increase an additional $3,200 than it does today.
Meanwhile, the cost of a colonoscopy at LCMC’s West Jefferson hospital would increase by nearly $1,700, and by more than $1,000 at Touro Hospital.
The cost of a colonoscopy at Lakeview Hospital, Lakeside Hospital and East Jefferson General Hospital would be approximately $3,800, nearly $3,200 higher than the average cost at an ambulatory surgical center in our network in the New Orleans area.

LCMC was allowed to acquire three hospitals in 2023 in accordance with the state’s Certificate of Public Advantage (COPA) process and is now demanding a more than 40% price hike for these facilities just two years later.
LCMC’s proposal for egregious price hikes is in direct contrast of the intention of the COPA, and is a perfect illustration of why the Federal Trade Commission (FTC) sued to stop LCMC’s acquisition of these three hospitals.
Under Louisiana’s COPA law, the certificate may not be issued unless the Attorney General’s office finds that “the agreement is likely to result in lower health care costs or is likely to result in improved access to higher quality health care without any undue increase in health care costs.”
Less than two years after the acquisition was allowed to go through, LCMC is now leveraging its market power to seek exorbitant cost increases that consumers and employers in Louisiana will bear the brunt of.
We have proposed rate increases that continue to reimburse LCMC at market-competitive rates while balancing access to affordable health care for the people and employers we serve.
We value the care LCMC provides to our members and want to keep them in our network. We are fully committed to continued good-faith negotiation with the goal of renewing our relationship at a cost that’s affordable and sustainable for consumers and local businesses.
Should we not reach an agreement, our number one priority is providing the people we serve continued, uninterrupted access to the care they need. UnitedHealthcare members who are in the middle of treatment at an LCMC hospital for a serious or complex condition are eligible for continuity of care.
Continuity of care provides continued in-network benefits for a period of time after a hospital leaves our network. Some examples of conditions eligible for continuity of care include but are not limited to:
- Patients who are pregnant
- People currently in active cancer treatment
UnitedHealthcare members must apply and be approved for continuity of care. They should call the number on their health plan ID card if they need assistance or have questions.
Our members will continue to have access to a broad network of hospitals throughout the New Orleans area should LCMC leave our network.
In the event LCMC leaves our network, we want our members to know they continue to have access to quality care in the New Orleans market. UnitedHealthcare members should call the number on their health plan ID card if they need assistance finding another provider in our network. They can also search our provider directory at myuhc.com.