Meeting market demands with enterprise-enabled agility
By choosing UnitedHealthcare, employers gain access to an enterprise with unparalleled scale, experience and resources to help meet their benefits goals.
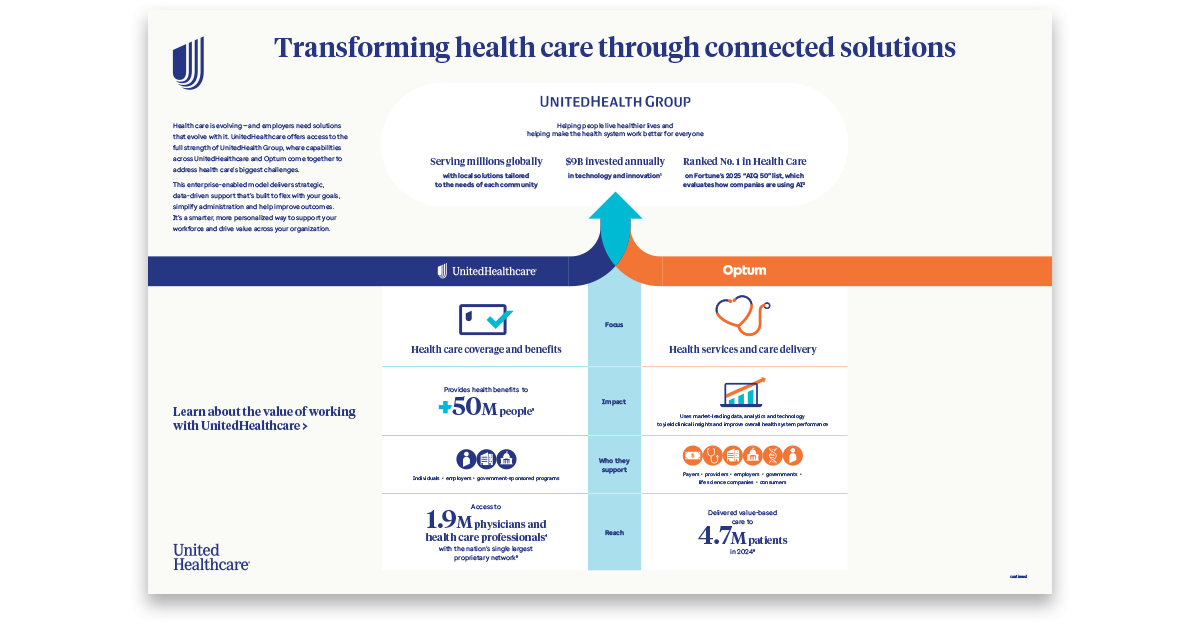
When clients work with UnitedHealthcare, they tap into the power of UnitedHealth Group — a global enterprise entrusted with providing health benefits and services to millions of members worldwide. UnitedHealth Group also includes Optum, a leading health solutions and care delivery organization.
UnitedHealth Group has been a leader in the charge to transform health care for more than a decade, investing $9B annually in technology and innovation.1 Its businesses — UnitedHealthcare and Optum — are laser-focused on delivering solutions that help people live healthier lives and help make the health system work better for everyone.
"At UnitedHealth Group, we recognize the profound challenges of the health care system," says Samantha Baker, chief growth officer for UnitedHealthcare Employer & Individual. "By harnessing the combined strengths of UnitedHealthcare and Optum, we are working toward innovative, sustainable solutions that can make a meaningful difference for the people we serve."
Each company brings its own unique capabilities to support this mission:
Transforming health care through connected solutions
Health care is evolving — and employers need solutions that evolve with it. UnitedHealthcare offers access to the full strength of UnitedHealth Group, where capabilities across UnitedHealthcare and Optum come together to address health care’s biggest challenges.
Offering unparalleled scale
UnitedHealth Group is powered by more than 400,000 people working every day to help ensure that people everywhere may access care with the goal of improving health outcomes and quality of life.
While the company has global reach, it takes a localized approach to meet the unique needs of each community and group it serves. This tailored strategy helps ensure that health care standards are advanced in every region — from urban cities to remote rural areas; for every employer group, from small family-run shops to large, geographically diverse organizations; and for every individual and family, regardless of income or circumstance.
This approach is reflected in UnitedHealth Group’s diverse portfolio of robust, market-leading health solutions. For instance, employer groups seeking pharmacy coverage can integrate their pharmacy benefits with UnitedHealthcare medical benefits for streamlined contracting, simplified benefits management and more coordinated care — potentially leading to better outcomes and cost savings. If that option isn’t the right fit for their organization or budget, Optum Rx® pharmacy services may be. The aim is to ensure employers, brokers and consultants don’t have to look far to assemble a competitive benefits package.
As a leading health care company, UnitedHealth Group is uniquely positioned to advocate on behalf of all the stakeholders and groups it serves. This includes collaboration with health systems, government entities, competitors and other health solutions companies — as well as brokers, consultants and employers — to address some of the industry’s most complex challenges and opportunities.
Bringing solutions for any client need
When a client approaches UnitedHealthcare with a challenge, sometimes the greatest value comes from an enterprise-enabled approach. UnitedHealthcare and Optum teams can deliver more strategic and tailored benefits packages aligned with the client’s specific goals.
The collaboration between UnitedHealthcare and Optum is central to this approach. Optum operates as the service provider for many UnitedHealthcare benefits and programs — from managing pharmacy benefits and coordinating behavioral health care to facilitating financing and payment of benefits. Additionally, some products and solutions are sold and serviced directly by Optum and may be the right fit for certain clients. This flexibility allows for a more agile response to the evolving needs of employers and their employees.
UnitedHealthcare provides robust health care solutions for employers, aligning services with employers’ business goals to help them manage employee benefits effectively. This approach works to support both employers’ business needs and their employees’ well-being.
By consolidating otherwise disparate solutions under one contract, UnitedHealthcare simplifies the administrative experience for employers — which may lead to greater financial savings and operational efficiency. Employees and their families also enjoy a more connected experience, with a single app or portal to access and manage their benefits.
As UnitedHealthcare continues to expand and enhance its portfolio — working across the enterprise to do so—it also sees value in helping to make it easier for employers and employees to find and purchase offerings that may extend beyond UnitedHealth Group. This is coming to life through UHC Hub®, which allows clients to select and purchase from a portfolio of selected vendors that may complement their existing UnitedHealthcare offerings. Additionally, UHC Store, available through the UnitedHealthcare® app, gives members the option to purchase discounted health and wellness offerings beyond their employer-sponsored benefits — at no extra cost to the client.
Collaborating across the company, and with others, enables UnitedHealthcare to unlock its full potential and solve clients’ needs more effectively.
Growing a national platform built for quality and affordable care
With a national network of over 1.9M physicians and health care providers and 5.6K hospitals,3 UnitedHealthcare has the country’s single largest proprietary network.4
But it’s not just about the numbers — UnitedHealth Group is leading the transition to value-based care, which aims to deliver better health outcomes at lower costs.
In 2024, for instance, Optum Health served approximately 4.7M patients through value-based care and continues to collaborate with over 100 health plans, including UnitedHealthcare, to help deepen patient engagement and enable earlier disease diagnosis.5 Patients under the care of Optum physicians in value-based care models — which are covered by most UnitedHealthcare networks — were 18% less likely to have an inpatient admission and 11% less likely to visit the emergency department compared to those in traditional fee-for-service plans.5
UnitedHealthcare Centers of Excellence (COEs), powered by Optum, are a network of quality medical facilities and providers that have demonstrated superior performance in specialized medical areas. These centers focus on treating complex conditions, such as organ transplants, congenital heart disease, cancer and bariatric surgery.
Each facility is rigorously evaluated annually by experts to ensure it meets strict criteria for maintaining its status in the network. These models are designed to enhance patient outcomes and help manage health care costs for both employees and employers.
“It’s important to ensure — no matter where a member is in the country, the plan offering they chose or how they are accessing care, whether in-person or virtual — that they receive the best available experience to support their condition,” says Jean-François Beaulé, executive vice president of design and innovation for UnitedHealthcare Employer & Individual. “UnitedHealthcare leverages a national proprietary platform using a common set of rules to integrate industry clinical standards to both augment providers’ knowledge when with their patient, as well as provide real-time information to help the member get the most out of their benefits and provide them with appropriate care recommendations."
Using its vast data to make a meaningful mark on the health system
UnitedHealthcare and Optum empower clients with the insights and resources they need to inform their benefits strategies and enable more personalized interactions and experiences for employees and their families.
For example, analysis of claims data may reveal opportunities for employers to further promote underutilized benefits, add new solutions to their benefits packages or better support a specific portion of their workforce. One UnitedHealthcare client, noticing high rates of type 2 diabetes among employees, added a diabetes management program to their plan — resulting in a 35% improvement in A1C levels over 12 months.7
UnitedHealthcare and Optum also use data to evaluate the effectiveness of their businesses, programs and solutions — identifying where administrative or care management improvements may be needed to better serve employers, members and providers. Data plays a key role in shaping the UnitedHealthcare consumer digital experience, including the responsible use of AI to help streamline and personalize experiences for members, providers, brokers, consultants and employers. These insights support more informed decisions that may lead to better health outcomes and more efficient processes.
Charting the course for change
UnitedHealth Group recognizes its role as a market leader and advocates for policies that support patients, providers and the health care industry. Understanding the significant impact it can have, the company strives to advance state and federal policies that enhance access and affordability for consumers and promote a more equitable, value-based health care system.
Collaborations with community organizations are central to UnitedHealth Group’s strategy for improving community health through targeted initiatives and programs. These collaborations are designed to address specific needs, such as chronic disease management, preventive care and health literacy. By working closely with community leaders and organizations, UnitedHealth Group can tailor its efforts to have the greatest impact, ensuring that resources are used efficiently and effectively. This grassroots approach not only strengthens the company’s presence in local communities but also underscores its dedication to making a tangible difference in people’s lives.
In addition, UnitedHealth Group’s commitment to consumer-centricity is helping to modernize health care experiences and address the pain points of working with and within the health system. To do this, UnitedHealth Group and its businesses are investing more than ever in technology to better serve those who rely on them. This synergy between consumer-centricity and technological advancement — backed by the strength and capabilities of an enterprise focused on making health care work better — has the potential to drive the transformation so many are eager to see.
At the heart of this effort is a deep sense of responsibility: to convene the right stakeholders and incite action that leads to meaningful change for the millions of people, companies and organizations it serves. It’s a responsibility UnitedHealth Group is honored to take on, feels best equipped to lead — and does not take lightly.